Safety in NHS services
 This document outlines some recent NHS initiatives aimed at maximising safety, whilst keeping quality of care at the centre of maternity services. This will help you understand how care is designed and how you can seek more support.
This document outlines some recent NHS initiatives aimed at maximising safety, whilst keeping quality of care at the centre of maternity services. This will help you understand how care is designed and how you can seek more support.
NHS Long Term Plan (2019) aims to:
- Improve access to support for mental health with the same urgency as physical health for birthing people, their partners and families. Look out for local information in the app or speak to your healthcare professional.
- Improve safety for baby through the NHS England Saving Babies’ Lives Care Bundle standards, by:
- 1. Offering choice and personalised care with respect for autonomy and decisions.
- 2. Offering support to reduce smoking.
- 3. Undertaking risk assessment and appropriate management of babies who might be at risk of growth restriction (slow growth).
- 4. Informing pregnant people of the importance of promptly reporting a reduction in baby’s movements.
- 5. Undertaking effective monitoring of the baby’s wellbeing during labour and birth.
- 6. Reducing the number of preterm births and optimising care when preterm delivery cannot be prevented through:
a) Prediction
- Undertake a risk assessment and refer to the low, intermediate or high-risk pathway and develop a personalised care plan for the birthing person.
b) Prevention
- Assess if aspirin is required from 12 weeks of pregnancy.
- Support to stop smoking.
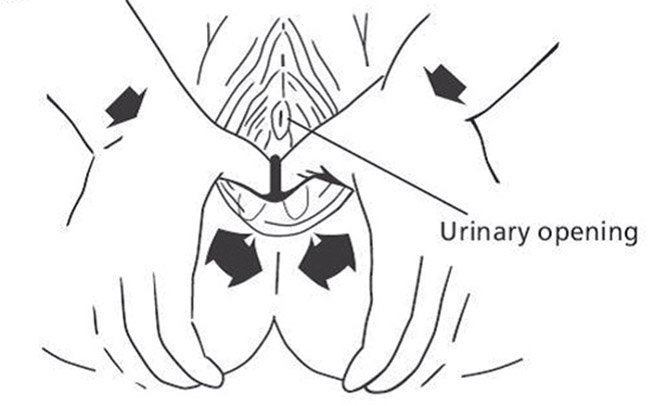
- Offer a urine test at the first antenatal appointment (Booking appointment) to screen for urine infection. If treatment is indicated, a repeat urine test should be taken to ensure infection has cleared up.
c) Preparation
- Optimise place of birth to ensure that birth occurs in a maternity unit that has the appropriate neonatal care services to support your baby.
- Birthing people are offered corticosteroid injections between 24 and 33+6 weeks, optimally at 48 hours before birth. This is to reduce the risk of your baby having breathing difficulties, gut problems, or bleeding in the brain.
- Birthing people who are in established labour, or who are having a planned preterm birth within the following 24 hours, are offered magnesium sulphate infusion between 24+0 and 29+6 weeks of pregnancy (or considered for this infusion between 30+0 and 33+6 weeks of pregnancy) to reduce the risk of cerebral palsy in babies.
- Improving general health outcomes for you and your baby. NHS England is funding a 6-8 weeks mother’s health check with your General Practitioner (GP)in addition to the baby check to assess your ongoing health and wellbeing needs.
Ockenden Report (2020)
This report aims to improve safety for you through pregnancy and post-birth through:- Enhanced safety in maternity units by undertaking a risk assessment at each contact with the birthing person to ensure that care is tailored to your needs.
- Maternity services must ensure that birthing people, their partners and their families are listened to.
- Care in complex pregnancies is managed with appropriate expertise and discussion and referrals made to specialist centres where necessary.
- Maternity services follow best practice in monitoring of the baby in labour.
- Provide access to accurate information to facilitate informed choice of intended place of birth and type of birth.
- Ensure there is access to translation services if communication in English is difficult.
Shared decision making
- All professionals should support you to make informed, value-based decisions by:
- introducing you to the options available, including their advantages and disadvantages
- helping you to explore these in the context of your preferences
- empowering you to make decisions – all professionals should support you to make informed, value-based decisions by:
- Ask yourself these three questions:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?