I’m pregnant …



 It may seem strange to be thinking about and planning contraception whilst you are pregnant. However, research has shown that many couples start having sex within six weeks of the birth of their baby. Did you know that it is possible to become pregnant when your baby is only 21 days old and before your menstrual period returns?
Effective, safe contraception is available at your maternity unit and can be started as soon as you give birth. This means you don’t need extra appointments at your GP or sexual health clinic to start contraception. This is particularly helpful at a time when you will be busy looking after a newborn baby and yourself.
Take some time to speak to your midwife or doctor about the options available to
you, some of which may be available immediately after the birth of your baby.
Planned pregnancies with an interval of at least one to two years are associated with a healthier pregnancy for you and your baby. Pregnancy spacing of greater than one year reduces the risk of pre-term birth, low birth weight and neonatal death. It also reduces the risk of complications in a future pregnancy particularly if you have given birth by caesarean section, because it allows the scar on your womb to fully heal.
Effective contraception puts you in control of deciding when and if you would like to have another baby and can have some beneficial effects on your periods and long term health.
You will be asked about your plans for contraception during antenatal appointments. Take some time to think about the different options and what might be right for you. Talk to your midwife or doctor and ask for any further information you may need. Once you have made a choice it can be entered into your personalised care and support plan and provided to you after birth.
It may seem strange to be thinking about and planning contraception whilst you are pregnant. However, research has shown that many couples start having sex within six weeks of the birth of their baby. Did you know that it is possible to become pregnant when your baby is only 21 days old and before your menstrual period returns?
Effective, safe contraception is available at your maternity unit and can be started as soon as you give birth. This means you don’t need extra appointments at your GP or sexual health clinic to start contraception. This is particularly helpful at a time when you will be busy looking after a newborn baby and yourself.
Take some time to speak to your midwife or doctor about the options available to
you, some of which may be available immediately after the birth of your baby.
Planned pregnancies with an interval of at least one to two years are associated with a healthier pregnancy for you and your baby. Pregnancy spacing of greater than one year reduces the risk of pre-term birth, low birth weight and neonatal death. It also reduces the risk of complications in a future pregnancy particularly if you have given birth by caesarean section, because it allows the scar on your womb to fully heal.
Effective contraception puts you in control of deciding when and if you would like to have another baby and can have some beneficial effects on your periods and long term health.
You will be asked about your plans for contraception during antenatal appointments. Take some time to think about the different options and what might be right for you. Talk to your midwife or doctor and ask for any further information you may need. Once you have made a choice it can be entered into your personalised care and support plan and provided to you after birth.
 These short videos have been designed to help those women and their partners who are unable to attend antenatal classes in person.
These short videos have been designed to help those women and their partners who are unable to attend antenatal classes in person.
 Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
 Altough rare, listeriosis infection in pregnancy can lead to miscarriage, stillbirth or severe illness in newborn babies. Listeria can be found in unpasteurised milk and in many chilled foods including pâté.
Altough rare, listeriosis infection in pregnancy can lead to miscarriage, stillbirth or severe illness in newborn babies. Listeria can be found in unpasteurised milk and in many chilled foods including pâté.

 Chest pain in pregnancy and/or afer your baby’s birth should never be ignored. Some chest pain can be serious and can lead to a heart attack, heart failure, cardiac arrest or even death. Most women do not suffer from these conditions during or after pregnancy but it is important to recognise the symptoms and, if you have any of them, to seek treatment quickly.
Chest pain in pregnancy and/or afer your baby’s birth should never be ignored. Some chest pain can be serious and can lead to a heart attack, heart failure, cardiac arrest or even death. Most women do not suffer from these conditions during or after pregnancy but it is important to recognise the symptoms and, if you have any of them, to seek treatment quickly.
 SCAD is a rare but serious heart condition that causes a tear or bruise to develop in a coronary (heart) artery resulting in a blockage that prevents normal blood flow. It can cause heart attack, heart failure or cardiac arrest and can be fatal.
SCAD can happen during pregnancy and during the weeks and months after you have given birth. Symptoms can include:
SCAD is a rare but serious heart condition that causes a tear or bruise to develop in a coronary (heart) artery resulting in a blockage that prevents normal blood flow. It can cause heart attack, heart failure or cardiac arrest and can be fatal.
SCAD can happen during pregnancy and during the weeks and months after you have given birth. Symptoms can include:




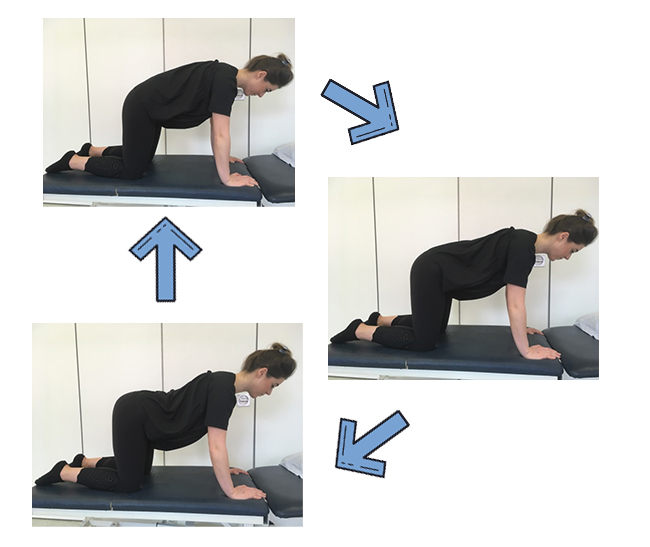
 You can also do this exercise lying on your side, or when sitting or standing.
You can exercise this muscle effectively when you are walking around or lifting and carrying. Just draw your tummy in as if you were hugging your bump or wearing a bikini!
You can also do this exercise lying on your side, or when sitting or standing.
You can exercise this muscle effectively when you are walking around or lifting and carrying. Just draw your tummy in as if you were hugging your bump or wearing a bikini!
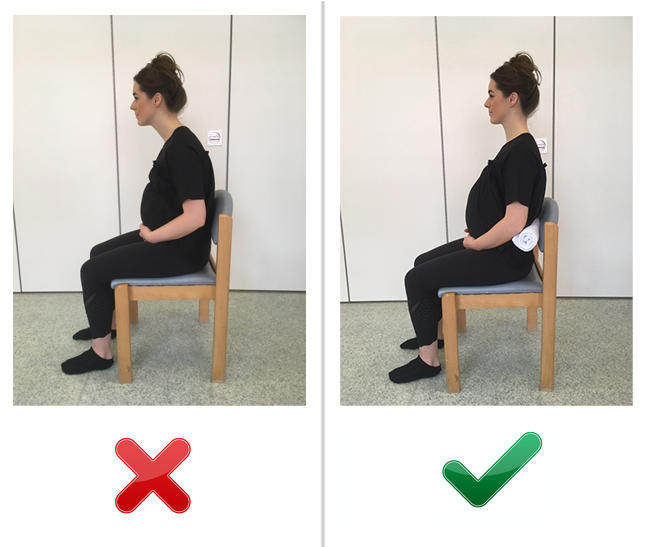
 Alternatively, you can try doing this exercise in different positions, such as when kneeling, leaning on the bed, sitting (on a chair or exercise ball), or on all fours) see pictures 1-2 and a-c).
Alternatively, you can try doing this exercise in different positions, such as when kneeling, leaning on the bed, sitting (on a chair or exercise ball), or on all fours) see pictures 1-2 and a-c).
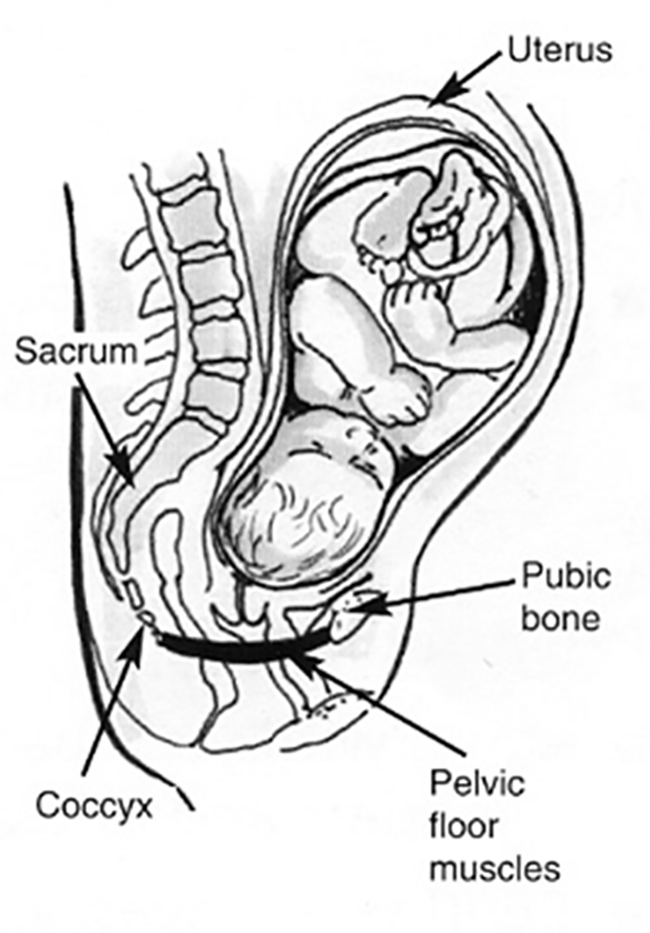 Some women may experience leakage of urine when coughing and sneezing (known as ‘stress urinary inconinence’) as a result of weak pelvic floor muscles. This is a common complaint affecting one in three women, but it can be prevented, reduced and even resolved fully with regular pelvic floor exercises.
It is highly recommended that all pregnant and postnatal women regularly exercise their pelvic floor muscles even if they have no problems with bladder control, to prevent problems in the future.
To begin with, you may have to concentrate while doing the exercises, but as you become more confident, you could do them whilst watching television, standing in a supermarket queue or waiting for the kettle to boil.
Some women may experience leakage of urine when coughing and sneezing (known as ‘stress urinary inconinence’) as a result of weak pelvic floor muscles. This is a common complaint affecting one in three women, but it can be prevented, reduced and even resolved fully with regular pelvic floor exercises.
It is highly recommended that all pregnant and postnatal women regularly exercise their pelvic floor muscles even if they have no problems with bladder control, to prevent problems in the future.
To begin with, you may have to concentrate while doing the exercises, but as you become more confident, you could do them whilst watching television, standing in a supermarket queue or waiting for the kettle to boil.
 Remember – it is not usually the one time we lift awkwardly or stand badly that causes pain; it is often the continual stresses and strains we place on our body during our everyday activities.
Therefore, it is important to modify your daily activities using the techniques in this booklet, do some of the gentle exercises we suggest and ensure you pace your activities throughout the day and week.
Please ask your midwife or GP to refer you to a physiotherapist if you are still having difficulties with pain.
Remember – it is not usually the one time we lift awkwardly or stand badly that causes pain; it is often the continual stresses and strains we place on our body during our everyday activities.
Therefore, it is important to modify your daily activities using the techniques in this booklet, do some of the gentle exercises we suggest and ensure you pace your activities throughout the day and week.
Please ask your midwife or GP to refer you to a physiotherapist if you are still having difficulties with pain.
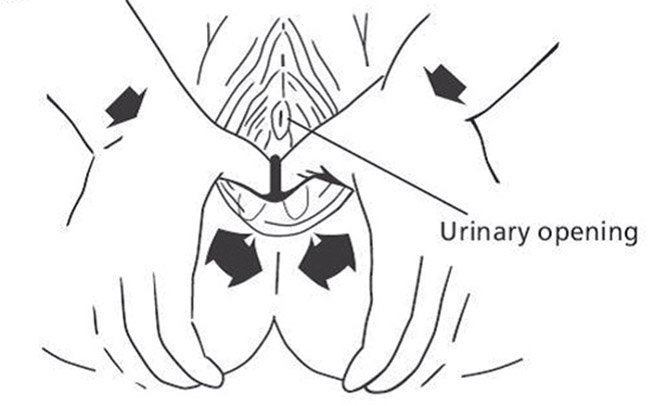
 Following this, apply a firm pressure at 5, 6 and 7 on the imaginary clock. Hold each stretch until you feel a burning, stinging sensation for approximately 2 minutes. This technique may be painful/cause stinging sensation – this is normal.
Try working in a circular montion with your thumb or fingertip across the scar and concentrate on one area of the scar at a time. Begin with a gentle pressure and build up as you feel comfortable.
Massage can also be performed in the bath without addition of any oils.
Following this, apply a firm pressure at 5, 6 and 7 on the imaginary clock. Hold each stretch until you feel a burning, stinging sensation for approximately 2 minutes. This technique may be painful/cause stinging sensation – this is normal.
Try working in a circular montion with your thumb or fingertip across the scar and concentrate on one area of the scar at a time. Begin with a gentle pressure and build up as you feel comfortable.
Massage can also be performed in the bath without addition of any oils.