Fibroids
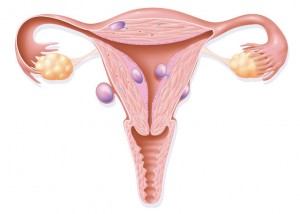 Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
- Fetal growth restriction (slow growth) – large fibroids may prevent a baby from growing well as there is less space in the womb.
- Placental abruption – this occurs when the placenta comes away from the wall of the uterus because it is blocked by the fibroid.
- Preterm birth – pain from fibroids may lead to uterine contractions, which can result in the baby being born early.
- Miscarriage – the presence of fibroids increases the risk of spontaneous miscarriage in early pregnancy.
- Caesarean birth – the presence of fibroids increases the need for caesarean birth due to the location of the fibroids in the womb. If the fibroids are located in the lower part of the uterus, they may block the opening of the birth canal resulting in the need for caesarean birth.
- Postpartum haemorrhage – poor contracting can lead to bleeding after the birth. If the uterus is unable to contract because of the presence of fibroids, the blood vessels that supplied the placenta may continue to bleed. Postpartum haemorrhage (bleeding) is a medical emergency and usually occurs 24-48 hours after birth. You should get help urgently.
Miscarriage and the loss of your baby: Frequently asked questions
Miscarriage and the loss of your baby: Frequently asked questions
I have been told I have an early miscarriage, what support can I get?
A miscarriage affects every woman and her partner differently. It can be a very distressing time and you may experience a range of emotions: a great sense of sadness, anger, guilt, loss and grief after the event. It is important to ensure that you get the emotional support you need to recover. This can be simply talking to family and friends, particularly someone who has also experienced a miscarriage. If you feel you are struggling to cope you should also speak to your GP for advice and support.Why has this happened to me?
Unfortunately, early miscarriages,(pregnancies lost within the first 12 weeks i.e. first trimester) are very common, 1 in 5 pregnancies. It is not always clear why a miscarriage has happened although the majority of these are thought to be due to abnormalities in the chromosomes (genetic material or DNA) that make up the pregnancy. These are usually random abnormalities that occur at conception meaning the baby is unable to develop normally. A poorly formed placenta can also cause problems. All these problems are unlikely to occur again, and the most likely outcome is that your next pregnancy will survive to birth. There are certain factors that increase the risk of miscarriage that you cannot control, such as getting older. However, medical conditions such as uncontrolled diabetes or thyroid disease, as well as lifestyle factors such as smoking, caffeine intake and your Body Mass Index (BMI) can also increase the risk. These factors can be controlled and it is worth seeing your GP for advice to optimise your chances of a healthy pregnancy in future.What happens next and what are my management choices?
In some miscarriages, the body recognises that the pregnancy has stopped developing and you start to bleed, which is often associated with tummy pain. For some women there are no symptoms and the diagnosis is only made during a routine ultrasound scan. Your choice of treatment option is guided by the type of miscarriage you have and the advice from your specialist on your personal circumstances.- If you miscarry early, the pregnancy may naturally and completely come away from the womb, so you have a “complete miscarriage”. This type of miscarriage does not need any treatment.
- An “incomplete miscarriage” is where a miscarriage has started but not all the pregnancy comes away, leaving some pregnancy tissue in the womb.
- A “missed (delayed) miscarriage” is where the baby has died in the womb and the mother often has no symptoms such as pain or bleeding.
- If you have an “incomplete”, “complete” or “missed (delayed) miscarriage” there are potentially up to 3 different management options available. These are:
- expectant (watching and waiting for the pregnancy to pass naturally)
- medical, or
- surgical management.
Expectant management
This involves watching and waiting to see if the pregnancy passes naturally. This option has the benefit of avoiding any form of intervention. Up to 50% of women may require further intervention later. It also may take some time (up to a few weeks) for the symptoms to start and bleeding can last up to 3 weeks. You will usually be advised to wait up to two weeks, but if you do not have any bleeding by then you may be offered either medication or surgery. The disadvantages of expectant management are the uncertainty of when bleeding will start and the anxiety while waiting. You may notice the pregnancy sac or the fetus being passed along with the blood clots. You will be carefully counselled by your specialist to make sure this option is the right one for you. You should ensure you have sanitary pads, pain relief and support at home to help you cope with managing the symptoms of miscarriage. Should you have any very heavy bleeding with large clots or pain that is not controlled with simple pain relief you should seek urgent medical attention and attend your nearest Accident & Emergency (A&E) department. You should have follow-up with your local Early Pregnancy Unit (EPU). Your EPU will normally arrange to see you again if you do not experience any significant bleeding or continue to bleed beyond 3 weeks, or develop a high temperature/flu-like symptoms. If your symptoms are consistent with having a miscarriage your EPU may ask you perform a urinary pregnancy test three weeks after the miscarriage, or attend for a repeat ultrasound scan to confirm if the miscarriage is complete.Medical management
This involves taking some medicine to encourage the miscarriage to start. You will need to insert a medication called misoprostol into the vagina (in some circumstances it can also be taken by mouth). Some EPUs offer women an oral pill first called mifepristone and then advise taking the vaginal medication 2 days later. This medication is successful in approximately 80-90% of women. The medication can sometimes cause some side effects including diarrhoea and nausea. You are likely to experience heavy bleeding with clots as well as cramping pain. Should you have very heavy bleeding with large clots or pain that is not controlled with simple pain relief you should seek urgent medical attention and attend A&E. You should inform your local EPU if you do not experience any significant bleeding within the first 48 hours after taking the misoprostol. You will be carefully counselled by your specialist to make sure this option is the right one for you. We recommend that you ensure you have some sanitary pads, pain relief and support at home to help you cope with managing the symptoms. The advantage of this type of management is that it speeds up the miscarriage whilst avoiding the risk of having surgical procedure. In some cases, the medicine is unsuccessful and women are then offered either a repeat tablet or surgery. There is also a small risk of some pregnancy tissue being left behind; most of the time this comes away naturally with the next period, but some women opt to have surgery to have this removed. You should have follow-up with your local early pregnancy unit (EPU). Your EPU will normally arrange to see you again if you do not experience any significant bleeding or develop a high temperature/ flu-like symptoms. If your symptoms are consistent with completing a miscarriage your EPU will ask you perform a urinary pregnancy test three weeks after the miscarriage. If your test is positive or continue to bleed 3 weeks after a miscarriage, you should inform your EPU so they continue to follow-up.Surgical management
This is what was traditionally known as a “D&C”. It involves gently opening (dilating) the cervix (neck of the womb) to allow a small suction tube to remove the pregnancy tissue from the womb. The tissue may be sent to the hospital lab for them to look at under the microscope to exclude any abnormal pregnancy tissue. You may be given medication prior to the procedure to soften the cervix allowing it to be opened up more easily This procedure can be done under a general anaesthetic (where you would be asleep) or under local anaesthetic known as an MVA (manual vacuum aspiration). This procedure takes approximately 20 minutes. Additional pain relief, such as tablets or “gas and air” (Entonox) may be recommended. The risks involved with surgical management include heavy bleeding, scarring (adhesions) in the lining of the womb and infection. There is a small risk that some pregnancy tissue remains within the womb which may come away naturally by itself or may require a further operation. The most serious possible complication is a making a hole through the womb, but this is very uncommon. After surgery, if your blood group is Rhesus negative, you should be offered an injection called Anti-D to prevent a condition called Rhesus Isoimmunisation. Rhesus isoimmunisation is where your body develops antibodies to your pregnancy because your blood group is different to that of your baby (i.e. your baby’s blood group is Rhesus positive). In future pregnancies the antibodies cross the placenta and attack the blood cells of your Rhesus positive baby; after surgery in early pregnancy Anti-D should be given to help prevent this happening.What worrying signs should I look out for?
After a miscarriage the bleeding should settle within about two to three weeks. If you are still bleeding after three weeks you should contact your local EPU. If you have any heavy bleeding, severe abdominal pain, fevers or offensive discharge you should contact your early pregnancy unit or attend your local A&E.What happens after the miscarriage?
Early miscarriages are very common and 1 in 5 women have a miscarriage for no obvious reason. This can be devastating and makes it psychologically harder to try again, as you want to understand why it happened and will it happen again. However, evidence shows most couples still go on to have a successful pregnancy even after two early miscarriages. If you have had three or more early miscarriages (seen in 1% of couples) your GP can refer you for tests and investigations by a specialist to try to understand why the miscarriages are happening and if treatments are available. Unfortunately, after all these investigations it may still not be possible to find out exactly why a miscarriage happened, which is so disappointing; this area is now subject to a lot of research to answer this question. However, despite this, it is still possible to have a successful pregnancy next time, especially if your investigations results are normal.When can I get pregnant again?
It is important that you wait until your follow up with the Early Pregnancy Unit (EPU) is complete. Your next period should normally come about 4-6 weeks after a miscarriage. Waiting for your next period before starting to try again to conceive is normally advised to help reset your body clock. It is also important to ensure you are emotionally as well as physically ready to embark on a new pregnancy. Emotional recovery often takes longer than your physical recovery.Deep vein thrombosis in pregnancy: Treatment
Deep vein thrombosis in pregnancy: Treatment
If you have been prescribed a treatment dose of blood thinning injections because you have been told that you have or may have a blood clot, here is some important information for you. Also read:Advice for you and staff caring for you
If you think labour has started or your waters have broken or you experience vaginal bleeding
Do not take further blood thinning injections and contact your maternity unit to arrange a review. Aim for vaginal birth on labour ward with spontaneous onset of labour.If the birth is planned as an elective caesarean section
Stop taking blood thinning injections 24 hours prior to planned operation date.If you require an induction of labour
Stop taking blood thinning injections 24 hours prior to admission for induction of labour. On admission, tell the midwife the time you took your last injection.In labour
All efforts will be made to reduce the time interval that you are without blood thinning injections, to help keep your blood clot risk low. On admission, inform the midwife the time you took your last injection. You will have medical and anaesthetic involvement during labour and induction of labour. Active management of the third stage of labour is recommended. For more information read: If postpartum haemorrhage (PPH) occurs, this will be managed by senior members of the maternity teamIf you are considering an epidural in labour
The safe time interval between blood thinning injections and having an epidural is at least 24 hours. This is to minimise the risk of bleeding. Inform staff the time of your last injection.After the birth
The dose will be restarted as soon as possible after the birth and will depend on your risk of bleeding.Duration of treatment after the birth
Treatment must continue for at least 6 weeks after the birth as the risk of blood clot is highest after the birth. The total duration will depend on when the treatment was started in pregnancy and must be at least 3 months. The maternity team will discuss the medication options before you go home. Switching to an oral anti-coagulation medication can be considered but this should be 5 days or more after birth. However direct oral anticoagulation medication is only an option if bottle feeding. Warfarin and LMWH are safe with breastfeeding.Follow up after hospital discharge
A clinic appointment with a specialist doctor will be arranged to provide you with guidance for the future, including the next pregnancy.Decide family planning method
Progesterone Only Pill (POP)/Implant/Intrauterine device/other. See here for more information: Also see: Contraceptive choices after you’ve had a babyUrgent concerns
Contact your maternity unit.Deep vein thrombosis in pregnancy: Prevention
Deep vein thrombosis in pregnancy: Prevention
If you have been told that you have a high chance of developing a blood clot during pregnancy and have been prescribed a PREVENTION dose of blood thinning injections, here is some important information for you. Also read:Advice for you and staff looking after you
If you think labour has started or your waters have broken or you experience vaginal bleeding
Do not take further blood thinning injections and make contact with your maternity team to arrange a review). Aim for vaginal birth on the labour ward with spontaneous onset of labour.If the birth is planned as an elective caesarean section
Stop taking blood thinning injections 12 hours prior to planned operation date (so the last dose should be at around 18.00 on the night before admission).If you require induction of labour
Stop taking blood thinning injections 12 hours prior to admission for induction of labour (so the last dose would be around 18.00 on the night before admission). On admission, tell the midwife the time you took your last injection.In labour
All efforts will be made to reduce the time that you are without blood thinning injections, to help keep your blood clot risk low. For the delivery of the placenta. active management is recommended. See here for more information: If postpartum haemorrhage (PPH) occurs, this will be managed promptly by senior members of the maternity team.If you are considering an epidural in labour
The safe time interval between blood thinning injections and having an epidural is at least 12 hours. This this is to minimise the risk of bleeding.After the birth
The injections will be restarted as soon as possible after the birth and will depend on your risk of bleeding.Duration of medication after the birth
Blood thinning injections must continue for at least 6 weeks after the birth as the chance of developing a blood clot is highest after the birth. Warfarin and LMWH are safe with breastfeeding. Switching to an oral medication may be considered after 5 days after the birth. However, direct oral anticoagulant therapy is only an option if you are bottle feeding your baby.Decide family planning method
Progesterone Only Pill (POP)/Implant/Intrauterine device/other. See here for more information: Also see: Contraceptive choices after you’ve had a babyUrgent concerns
Contact your maternity unit.Deep vein thrombosis (DVT) in pregnancy: Frequently asked questions
Deep vein thrombosis (DVT) in pregnancy: Frequently asked questions
How is the diagnosis made?
At your initial appointment with the midwife, periodically through the pregnancy and after your baby is born you will be risk assessed for your personal chance of developing a venous thromboembolism (DVT). All women will be recommended to keep hydrated and mobile during pregnancy, labour and birth. Those in groups with a medium to high chance of developing a DVT may have additional care recommended to them. Interventions during labour and birth, such as assisted vaginal birth or caesarean birth increase your chances of developing DVT.What does this mean?
For Me
Women who have a higher chance of developing DVT during pregnancy may be recommended to take a medication during pregnancy and the postnatal period to reduce this chance. The medication is a daily injection of a blood thinning medication (low molecular weight heparin) which you will be taught how to administer to yourself. Your partner or family member can be taught how to give the injection to you if you prefer. In addition you may be given compression stockings, to wear when you are admitted to hospital.For my baby
The low molecular weight heparin injections do not cross the placenta and your baby will not be affected by their use.What symptoms and signs should I be looking out for?
If you develop any swelling or pain in your legs or chest pain or difficulty in breathing you should attend the maternity unit for review as soon as possible.How may this impact my birth choices?
If you are taking a preventative dose of low molecular weight heparin during pregnancy, there needs to be a 12 hour window between your last injection and the siting of an epidural (pain relief). So if your labour is starting or your waters have broken and a dose of the medication is due, please speak to your midwife or obstetrician first.How may this affect care after the birth?
Women who are at a higher chance of developing a DVT might be recommended to have low molecular weight injections for ten days or six weeks after their baby is born.What will this mean for future pregnancies? How can I reduce my risk of this happening again?
Depending on the reasons you have an increased chance of DVT, these reasons are likely to occur in any future pregnancy.Where can I find out more information about this condition?
Reducing the risk of venous thrombosis in pregnancy and after birthPlacenta praevia: Frequently asked questions
Placenta praevia: Frequently asked questions
How is the diagnosis made?
The location of your placenta is identified at your mid-pregnancy anomaly ultrasound scan. If the placenta is covering the neck of the womb it is termed a placenta praevia; if it is not covering the neck of the womb but is within 20mm of the neck of the womb it is called a low lying placenta. The location of the placenta will be checked again closer to the end of the pregnancy, usually at around 36 weeks. 9 out of 10 women will not have a low lying placenta or placenta praevia at their follow up scan.What does this mean?
For me
Having a low lying placenta or placenta praevia increases the chance of experiencing bleeding during pregnancy. A planned caesarean birth will be recommended to all women with a low lying placenta or placenta praevia towards the end of pregnancy.For my baby
If there is extremely heavy vaginal bleeding during pregnancy from a low lying placenta or placenta praevia, this may affect your baby’s wellbeing. A baby may need to be born prematurely if a woman experiences extremely heavy vaginal bleeding during pregnancy. If you experience any vaginal bleeding, contractions or pain you should attend hospital without delay.What are the ‘red flag’ symptoms/concerns, which means that they should be reported immediately?
If you experience any vaginal bleeding, contractions or pain you should attend hospital without delay.How may this impact my birth choices?
A planned caesarean birth will be recommended to all women with a low lying placenta or placenta praevia towards the end of pregnancy. Heavy bleeding is possible during the caesarean birth, and this may require a blood transfusion and medications to limit the blood loss. Rarely, if there is no other way to control the bleeding, it may be necessary to remove your womb (hysterectomy) at the time of a caesarean birth for a low lying placenta or placenta praevia.What will this mean for future pregnancies? How can I reduce my risk of this happening again?
A low lying placenta or placenta praevia is associated with previous caesarean birth, assisted reproductive technologies and smoking.Mental health and wellbeing concerns: Frequently asked questions
Mental health and wellbeing concerns: Frequently asked questions
How is the diagnosis made?
This was made before pregnancy. Ideally all women with mental health concerns/issues should be offered preconception counselling to optimise their health before pregnancy. Your GP will notify the maternity team however it is wise for you to tell your midwife at the first appointment (Booking appointment) so that the appropriate support can be put in place for you.What does this mean?
For me:
You are at risk of your mental health worsening during pregnancy. If there is a family history of mental health you are at more risk of worsening mental health during pregnancy. It is really important that you tell your midwife if you are feeling mentally unwell and give your family permission to inform the maternity team too.For my baby:
Your baby can be at risk if you do not look after yourself.What will the medical team recommend?
You should ask to speak to someone as soon as possible if you feel your mental health is worsening.What tests will/may be considered? How often may they be needed?
Depending on your level of need you will be cared for by the local perinatal mental health team, who may make specialist referral for you.What are the ‘red flag’ symptoms/concerns, which means that they should be reported immediately?
Low mood and feeling hopeless, helpless or isolated.How are recommendations made regarding?
Treatment options
We can offer counselling or medication. Many medications are safe in pregnancy. If you are taking medication prior to pregnancy you should discuss your ongoing treatment with your GP and medical team before making any changes.How may this affect care after the birth?
A birth plan prior to birth should be agreed with you to ensure there is a safe plan for you and your baby after birth.What will this mean for future pregnancies? How can I reduce my risk of this happening again?
Optimise your mental health and symptoms between pregnancies.What will this mean for future/my long-term health and how can I influence this?
Contraception and a follow up plan should be made to optimise your health for future pregnancies. This may include well-being and medication review.Pregnancy sickness: Frequently asked questions
Pregnancy sickness: Frequently asked questions

What does this mean for me?
Nausea and vomiting are common symptoms of pregnancy and affects 8 in 10 women. It usually starts early in pregnancy and resolves by the end of the first trimester, although in some cases it can last for longer. Some women have more severe symptoms, particularly if:- they had it before: or
- are having multiple pregnancy like twins or triplets; or
- an uncommon condition known as a molar pregnancy.
What is Hyperemesis Gravidarum (HG)?
This a severe form of nausea and vomiting in pregnancy, where you become dehydrated, lose a significant amount of weight, and have abnormal blood tests. It may affect 1 to 3 in 100 pregnant women. Women with this condition may need to be attend hospital for rehydration. For many women, HG settles by 20 weeks (5 months) but occasionally it can last until the end of pregnancy. Nausea and vomiting of pregnancy can sometimes affect your mood and all aspects of your normal day and home life. In some women, the symptoms can be so severe that they become depressed and need extra support such as counselling. If you find that you persistently feel down then you should seek help and speak to your GP, midwife or local Early Pregnancy Unit (EPU).What treatment do I need?
Most women with mild symptoms will be able to manage their symptoms themselves. You should eat small amounts often and avoid any foods or smells that trigger symptoms. Some women find eating or drinking ginger products helps. Complementary therapies such as acupressure or acupuncture may also be helpful. If this does not help, you should see your GP, who will prescribe anti-sickness medication. These are safe to take in pregnancy. If your symptoms do not settle despite oral anti sickness medication, and you have any of the following symptoms, you should attend your local Accident and Emergency (A&E) department or speak to the EPU at your local hospital:- You are not able to tolerate any food or water.
- You feel dehydrated (thirsty, dry mouth, dark urine).
- You have lost weight (losing 5% or more of your pre-pregnancy weight is a concern).
- You have fever, blood in your vomit, abdominal pain, or loose stools.
- You have a medical condition which requires you to take tablets you can no longer take due to vomiting e.g anti-epileptic drugs.
- You have a medical condition such as a heart or kidney problem or diabetes.
What will this mean for future pregnancies?
You are at a higher risk of developing this in future pregnancies, so do seek help early if you find that you are struggling with your symptoms.Where can I find out more information about this condition?
Pregnancy sickness and Hyperemesis Gravidarum
Pregnancy sickness and Hyperemesis Gravidarum

What is pregnancy sickness?
Normal pregnancy sickness is short spells of nausea and occasional vomiting usually during the early stages of pregnancy. It is common in many pregnancies, normally beginning around 4-6 weeks and eases between 12-20 weeks. It can affect you at any time of the day or night, and some people feel sick all day long. It is usually well managed through diet and lifestyle changes. In general, there are no bad physical or mental side effects as it’s a normal part of pregnancy.Coping strategies
If your sickness isn’t too bad, you can try some lifestyle changes:- Get plenty of rest as tiredness can make nausea worse.
- Avoid foods or smells that make you feel sick.
- Eat dry toast or a plain biscuit before you get out of bed.
- Eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta).
- Eat cold foods rather than hot ones if the smell of hot meals makes you feel sick.
- Drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting).
When to seek help
- When your quality of life is being affected and you’re not able to manage your usual activities
- If your symptoms are much worse than you were expecting them to be
- If you are not keeping down any food or drink, or only a very small amount
- If you’ve lost weight
- If you have signs of dehydration such as dry mouth, dry lips, headaches or feel dizzy, weak or confused. Changes in urine (wee) being darker, not going as much or only weeing a small amount.
What is Hyperemesis Gravidarum?
Hyperemesis Gravidarum (HG) is severe sickness and nausea in pregnancy where medical treatment and emotional support is needed. It can lead to a lot of weight loss and dehydration. Around 10,000-20,000 pregnancies a year are affected by this condition. It can start very early, even before a positive pregnancy test. Symptoms are usually the worst at 9-13 weeks, and get a bit better around 16-24 weeks, but it can go on all the way through the pregnancy for some people.When to seek help
If you are being sick often and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and it is important you get the right treatment as soon as possible. You should always seek help if you suspect you have HG, or severe nausea and vomiting, or if you have any of the following symptoms:- Prolonged or constant nausea and/or vomiting affecting your day-to-day activities, like being about to go to work, look after your home or other children, or look after yourself.
- You have signs of dehydration, such as a dry mouth, dry lips, headaches, dizziness, weakness, feeling confused. If your wee changes, for example if it is darker, you are not going as much, passing only a small amount.
- If you’ve lost weight, this could be an indicator of HG.
- Your symptoms are affecting your mental health and you are struggling to cope. If you have had HG before, unfortunately, it’s likely you will get it again in another pregnancy. If you decide on another pregnancy, it can help to plan ahead, such as arranging childcare so you can get plenty of rest. Talk to your GP about starting medicine early. Medication can be prescribed before symptoms even begin.
Other symptoms of HG:
- Sensitive to smells
- Excessive saliva production
- Headaches and constipation from dehydration
- Loss of bladder control
- Tiredness
- Acid reflux
- Sensitive to lights/noise/movement
Coping strategies
- Rest! There may be times where symptoms have eased and you feel like you can do more, but it’s important to still rest as much as possible.
- Avoid triggers of nausea as much as possible. If that means avoiding cooking and being as far away from the kitchen as possible while someone else is cooking, then that is what you must do. It’s okay to ask that your family, colleagues or friends avoid certain foods whilst you are around them. Other sensory stimulation such as noises, moving, screens, or bright lights may be triggers too and should be avoided if they make your symptoms worse.
- Try to avoid getting dehydrated. If drinking triggers vomiting or nausea, then sucking ice cubes made of juice or drinking very slowly through a straw may be the only way to stay hydrated. Bottled water may taste better than tap water. If you can’t keep fluids down, then be prepared for a hospital admission to have fluids through a drip. This is vital for you and your baby’s health and can make you feel much better.
- Keep a diary. Tracking your food and drink intake will be helpful for the doctor to assess what treatment you need and for you to see if you have any food triggers. Tracking your symptoms may show a pattern and show you when is the best time to eat. It can also help you prepare for when you know your symptoms will be worse.
Hyperemesis Gravidarum treatments
Hyperemesis Gravidarum treatments





