Oral health and eye care in pregnancy

Oral health in pregnancy
During pregnancy and after birth it’s important to have regular dental check-ups.
NHS dental care is free for pregnant women and for one year after the birth or the expected first birthday of your baby. It is recommended that all pregnant women see their dentist during pregnancy. It is especially important to see your dentist if you have persistent sore or bleeding gums.
Hormonal changes in pregnancy may cause bleeding gums. It is important to keep a good level of dental hygiene to prevent tooth decay and gum disease. It is recommended that you brush twice a day with fluoride toothpaste containing at least 1350 ppm fluoride (this is safe to use in pregnancy).
Try to limit the amount of sugary food and drink you eat and then keep them for mealtimes rather than as snacks.
Remember to wait to brush your teeth after eating for at least 1 hour. This will prevent further dental erosion.
Eye care in pregnancy
During pregnancy you may experience slight changes in your vision and/or dry eyes. Eye tests are recommended every two years. Eye tests are free if you are on social benefits. Contact your local optician to book an appointment.
Your GP can provide you with a signed form for a maternity exemption certificate. This will entitle you to free NHS prescriptions up to one year after the birth of your baby, and free NHS dental care.
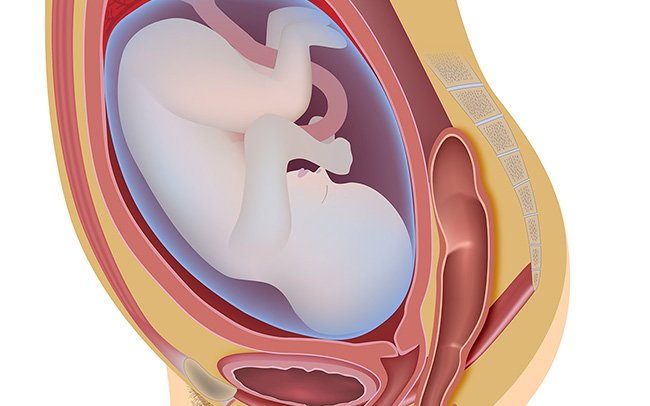
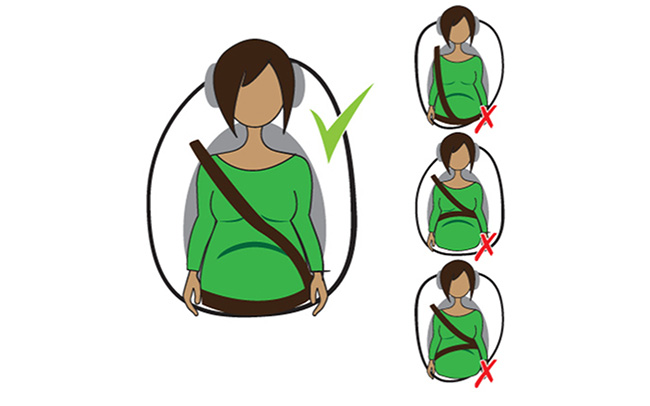 On long car journeys it is important to stop regularly for a break and to stretch your legs. Wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump. Road accidents are among the most common causes of injury in pregnant women. Avoid making long trips on your own and share the driving with others when possible.
On long car journeys it is important to stop regularly for a break and to stretch your legs. Wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump. Road accidents are among the most common causes of injury in pregnant women. Avoid making long trips on your own and share the driving with others when possible.