Breast changes
 The milk that your breasts first produce is called colostrum, and this will be present in the breast from mid-way through your pregnancy. Colostrum helps protect your baby from allergies and disease. Colostrum is concentrated breastmilk that comes in tiny amounts which is sufficient for the baby for the first three days.
Around three days after birth, the colostrum changes and becomes mature milk – and this change may make your breasts feel heavy and tender.
Engorgement is common and can happen when your milk “comes in” or if your breasts become over full of milk, especially when your baby is not latched on to the breast effectively. Engorgement can be relieved with frequent breastfeeding. If your breasts feel so full that your baby is unable to take the breast, try hand expressing a little of your milk before attempting to latch baby to the breast. See How to hand express.
If your breasts are not relieved by feeding and hand expressing, seek help urgently. See Help with breastfeeding.
Engorged breasts can progress to mastitis rapidly. Mastitis is an infection that can occur when milk ducts become blocked. Additional symptoms include a high temperature, and or lumps in your breasts that are hot, red and painful.
The milk that your breasts first produce is called colostrum, and this will be present in the breast from mid-way through your pregnancy. Colostrum helps protect your baby from allergies and disease. Colostrum is concentrated breastmilk that comes in tiny amounts which is sufficient for the baby for the first three days.
Around three days after birth, the colostrum changes and becomes mature milk – and this change may make your breasts feel heavy and tender.
Engorgement is common and can happen when your milk “comes in” or if your breasts become over full of milk, especially when your baby is not latched on to the breast effectively. Engorgement can be relieved with frequent breastfeeding. If your breasts feel so full that your baby is unable to take the breast, try hand expressing a little of your milk before attempting to latch baby to the breast. See How to hand express.
If your breasts are not relieved by feeding and hand expressing, seek help urgently. See Help with breastfeeding.
Engorged breasts can progress to mastitis rapidly. Mastitis is an infection that can occur when milk ducts become blocked. Additional symptoms include a high temperature, and or lumps in your breasts that are hot, red and painful.
If you are experiencing symptoms of mastitis contact your midwife, GP or the maternity triage/assessment centre where you gave birth urgently.
Backache
 It is not uncommon to experience backache after the birth, particularly if you have had an epidural in labour. This is completely normal and should resolve in time with rest, warms baths and mild analgesia. If pain continues, speak to your midwife or doctor.
See the POGP Fit for Future booklet in the related link for tips on how to manage back pain after birth.
It is not uncommon to experience backache after the birth, particularly if you have had an epidural in labour. This is completely normal and should resolve in time with rest, warms baths and mild analgesia. If pain continues, speak to your midwife or doctor.
See the POGP Fit for Future booklet in the related link for tips on how to manage back pain after birth.

Opening your bowels

How to manage your bowels
Many women are anxious about opening their bowels for the first time after delivery, especially if they have had stitches. It is important that you try not to put off opening your bowels once you have had the urge to go, as this can make you more constipated.
If you have been prescribed laxatives please use these as you will need to ensure that your stools remain soft but not watery. It is important to keep your stools like a ‘toothpaste’ consistency.
To help prevent constipation you will need to maintain a good fluid update (2.5-3 litres if breastfeeding) and a healthy diet rich in fibre.
Make sure you sit in a good position on the toilet to ensure you completely empty your bowels. The ideal position is:

- knees higher than your hips (to do this place your feet on a step or point your toes)
- lean forward and put yuor elbows on your knees
- bulge your abdomen outwards as you take a breath in and straighen your spine
- if you have discomfort, or are worried about the stitches you can hold a sanitary pad or a wad of tissues with your hand and apply pressure to the vagina and perineum
Piles (haemorrhoids)
Piles are swellings of the blood vessels inside or around the rectum, and are very common following pregnancy and birth. In most cases, piles will disappear without treatment within a few weeks of birth. Ask your midwife, doctor or local pharmacist for advice regarding piles if you think you may have them, or if they become painful.

Passing urine

Taking care of your bladder
After delivery, your midwife will give you a bowl to measure your urine in. It is important for your midwife to know the volume of urine to ensure your bladder is working properly.
You may have a catheter post-delivery. After the catheter is removed it is important that you pass urine within six hours. If you don’t, you must tell your midwife or doctor immediately.
If you are having difficulty passing urine or have not had an urge to pass urine four hours after your catheter has been removed try:
- going to sit on the toilet, relaxing and leaning forwards
- turning on the taps so you can hear running water or pulling lightly on the pubic hair (both of these can help to stimulate an urge)
- rocking forwards and backwards on the toilet
- gently tapping over the bladder near your pubic bone for a few minutes
After birth, some women find that their bladder function is not as efficient and can experience:
- urinary retention (when the urge to pass urine is absent or isn’t as strong – this leads to the bladder overfilling. This over-stretching can cause long-term damage to the bladder)
- stress urinary incontinence (when urine leaks on sneezing, coughing or exercising)
- urgency urinary incontinence (when you suddenly need to pass urine with no prior sensation to do so – leading to leaking of urine).
Pelvic floor exercises can help improve bladder function, however if you are worried about your urinary control, or any symptoms of bladder dysfunction persist it’s important to speak to your midwife, health visitor or GP.

Bleeding
 Some bleeding after birth is normal – this is recorded in your notes as estimated blood loss (EBL).
Vaginal bleeding after birth is referred to as lochia, which is a mix of blood and other products from inside the uterus. This can be quite heavy at first, requiring several sanitary pad changes a day. After the first week the lochia slows down and becomes pink/light brown in colour. This loss will normally disappear by four weeks after birth.
Any large clots, silky membranes, sudden heavy bleeding or an offensive smell may be a sign that something is wrong and should be discussed with your midwife or GP urgently.
Some bleeding after birth is normal – this is recorded in your notes as estimated blood loss (EBL).
Vaginal bleeding after birth is referred to as lochia, which is a mix of blood and other products from inside the uterus. This can be quite heavy at first, requiring several sanitary pad changes a day. After the first week the lochia slows down and becomes pink/light brown in colour. This loss will normally disappear by four weeks after birth.
Any large clots, silky membranes, sudden heavy bleeding or an offensive smell may be a sign that something is wrong and should be discussed with your midwife or GP urgently.
Retained products
You may be aware that when the placenta detaches from the inside of the uterus sometimes small pieces or fragments are left behind. Your midwife will have checked the appearance of the placenta to check whether there are any obvious pieces missing, but it is not always possible to spot fragments that have been left behind. The same is true when a caesarean is performed. Even though the doctors will have checked the inside of the uterus for any remaining placenta, it is not always possible to identify them.
For most women, any retained fragments of placenta (sometimes referred to as “retained products”) will pass unnoticed with the normal lochia in the days or weeks following the birth. However, for a small number of women, retained products that do not pass naturally may require medical assistance. It may be that heavy bleeding occurs, or you begin passing blood clots. Or you may develop a temperature and feel shivery and unwell. These are potential signs of retained products that require treatment and if you develop any of these symptoms, you should get in touch with your local maternity Triage, or see your GP.
Occasionally the retained products require surgical removal. This will involve a short procedure under a general anaesthetic, but most women can go home the same day.
Common physical concerns after birth
 Find out more about how your body may feel after birth and how to support your physical recovery by exploring the links below.
Find out more about how your body may feel after birth and how to support your physical recovery by exploring the links below.

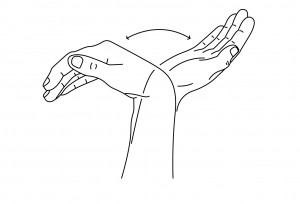
 During pregnancy, the body naturally retains more fluid, and swelling of the hands is common. If some of this fluid is localised to the carpal tunnel, this leads to pressure on the median nerve causing the symptoms of CTS. Up to 62% of pregnant women develop CTS. These symptoms are also common after the birth.
During pregnancy, the body naturally retains more fluid, and swelling of the hands is common. If some of this fluid is localised to the carpal tunnel, this leads to pressure on the median nerve causing the symptoms of CTS. Up to 62% of pregnant women develop CTS. These symptoms are also common after the birth.
 2. Hand squeeze. Make a release a fist (this can be done with your hands elevated). You could also squeeze a stress ball:
2. Hand squeeze. Make a release a fist (this can be done with your hands elevated). You could also squeeze a stress ball:
 3. Fingers bend and straighten. Forearm upright, wrist and fingers straight. Now hook your fingers down, trying to touch the tips of your fingers to the top of your palm. Straighten again. Repeat 10 times:
3. Fingers bend and straighten. Forearm upright, wrist and fingers straight. Now hook your fingers down, trying to touch the tips of your fingers to the top of your palm. Straighten again. Repeat 10 times: