Placenta praevia: Frequently asked questions
How is the diagnosis made?
The location of your placenta is identified at your mid-pregnancy anomaly ultrasound scan.
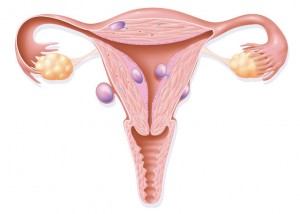
If the placenta is covering the neck of the womb it is termed a placenta praevia; if it is not covering the neck of the womb but is within 20mm of the neck of the womb it is called a low lying placenta.
The location of the placenta will be checked again closer to the end of the pregnancy, usually at around 36 weeks. 9 out of 10 women will not have a low lying placenta or placenta praevia at their follow up scan.
What does this mean?
For me
Having a low lying placenta or placenta praevia increases the chance of experiencing bleeding during pregnancy.
A planned caesarean birth will be recommended to all women with a low lying placenta or placenta praevia towards the end of pregnancy.
For my baby
If there is extremely heavy vaginal bleeding during pregnancy from a low lying placenta or placenta praevia, this may affect your baby’s wellbeing.
A baby may need to be born prematurely if a woman experiences extremely heavy vaginal bleeding during pregnancy.
If you experience any vaginal bleeding, contractions or pain you should attend hospital without delay.
What are the ‘red flag’ symptoms/concerns, which means that they should be reported immediately?
If you experience any vaginal bleeding, contractions or pain you should attend hospital without delay.
How may this impact my birth choices?
A planned caesarean birth will be recommended to all women with a low lying placenta or placenta praevia towards the end of pregnancy.
Heavy bleeding is possible during the caesarean birth, and this may require a blood transfusion and medications to limit the blood loss. Rarely, if there is no other way to control the bleeding, it may be necessary to remove your womb (hysterectomy) at the time of a caesarean birth for a low lying placenta or placenta praevia.
What will this mean for future pregnancies? How can I reduce my risk of this happening again?
A low lying placenta or placenta praevia is associated with previous caesarean birth, assisted reproductive technologies and smoking.

Deep vein thrombosis in pregnancy
 Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
Signs/symptoms
- Pain/tenderness in the leg behind the knee or in the calf.
- Feeling of heat in the affected area or a red discolouration of the skin.
- Swelling of the affected area.
- A pulmonary embolism may cause shortness of breath and chest pain, which comes on suddenly and worsens with deep breaths, coughing or chest movement.
If you have any of these symptoms you should speak to a health professional immediately, or attend your local A&E department.
Treatment
These conditions are serious and will require urgent treatment in hospital with medications that prevent the clot from getting bigger and breaking off and travelling to another part of the body.
Prevention
- Keep mobile and rotate your ankles regularly.
- Wear compression stockings if your midwife or doctor have advised you to do so.
- Consider taking short walks when you feel up to it.
- Stay well hydrated.
- Avoid sitting/lying down for prolonged periods, ie, in a car/on a train.
Staff use a venous thromboembolism risk scoring system at your Booking appointment to determine your risk during pregnancy. Read the related links to find out what conditions can increase the risk of a DVT during pregnancy.
 During pregnancy your midwife or doctor will be checking to ensure that your baby is growing well. This is done at defined stages in the pregnancy, either by measuring your bump with a tape measure or by routine ultrasound scans. If there is a concern about the growth of your bump you may be referred for a growth scan. Your baby’s progress is plotted on a chart by the person taking the measurement (midwife, doctor or sonographer).
If your baby is found to be growing smaller than expected you may require additional ultrasound scans and antenatal appointments to monitor your baby’s wellbeing.
During pregnancy your midwife or doctor will be checking to ensure that your baby is growing well. This is done at defined stages in the pregnancy, either by measuring your bump with a tape measure or by routine ultrasound scans. If there is a concern about the growth of your bump you may be referred for a growth scan. Your baby’s progress is plotted on a chart by the person taking the measurement (midwife, doctor or sonographer).
If your baby is found to be growing smaller than expected you may require additional ultrasound scans and antenatal appointments to monitor your baby’s wellbeing.