Birth registration
 Following the arrival of your baby, the birth needs to be registered within 42 days (six weeks) at your local registry office. It is through this process that you will obtain a birth certificate.
The registration should be done in the borough you gave birth in. You may register the birth in a different area if this is more convenient, however your details will need to be sent to the borough in which you gave birth in order for them to generate a valid birth certificate.
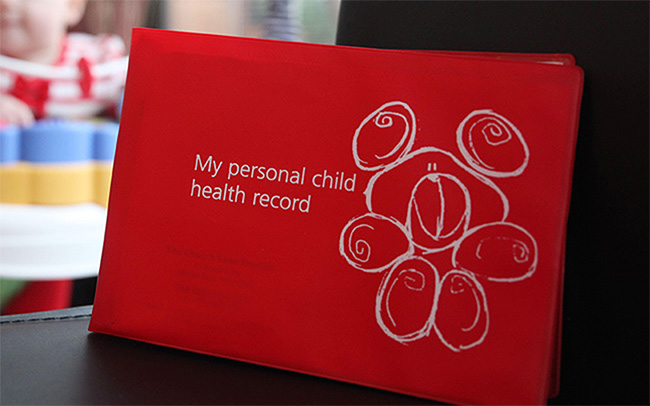
The service is normally provided by appointment only, but this may vary from one area to the next. Please take the Personal Child Health Record (red book) and your baby’s NHS number with you, as the registrar may ask to see it.
Following the arrival of your baby, the birth needs to be registered within 42 days (six weeks) at your local registry office. It is through this process that you will obtain a birth certificate.
The registration should be done in the borough you gave birth in. You may register the birth in a different area if this is more convenient, however your details will need to be sent to the borough in which you gave birth in order for them to generate a valid birth certificate.
The service is normally provided by appointment only, but this may vary from one area to the next. Please take the Personal Child Health Record (red book) and your baby’s NHS number with you, as the registrar may ask to see it.
Portal: Birth registration for your region
 Following a caesarean you may feel sore and swollen for a few days. To help with pain, regular pain relief is recommended in combination with early and gentle movement.
Always wash your hands before caring for your caesarean wound.
Your scar will take up to six weeks to heal, and to assist with healing you should:
Following a caesarean you may feel sore and swollen for a few days. To help with pain, regular pain relief is recommended in combination with early and gentle movement.
Always wash your hands before caring for your caesarean wound.
Your scar will take up to six weeks to heal, and to assist with healing you should: