Giving birth to your breech baby: Frequently asked questions
How is the diagnosis made?
It may be suspected that your baby is lying feet or bottom first in the womb, when a midwife or obstetrician feels your abdomen at or after 36 weeks of pregnancy. This is then usually confirmed by an ultrasound scan. If you are in labour when this is suspected, the baby’s position may be confirmed by internal examination.What will the medical team recommend?
When a baby is in a breech position after 36 weeks of pregnancy there are three options that might be possible: 1. An external cephalic version (ECV) – using pressure on your abdomen to turn the baby head first 2. A planned vaginal breech birth 3. A planned caesarean birth If the breech position is first noted during labour an ECV may not be possible, and a woman will need to choose between a vaginal breech birth and a caesarean birth.What tests will/may be considered? How often may they be needed?
An ultrasound to check on the growth of your baby may be arranged if the breech position is detected before labour. This can help to guide your decision making about your preferred mode of birth.What symptoms and signs should I be looking out for?
You should contact your maternity unit if you think your waters have broken or you are in labour with a baby known to be in the breech position.What are the ‘red flag’ symptoms/concerns, which means that they should be reported immediately?
If your waters break and your baby is lying feet or bottom first, there is an increased chance of the umbilical cord being below the baby – this is called an umbilical cord prolapse. If this happens you should promptly attend the hospital for review. If a loop of cord is seen outside the vagina, then you should call 999 immediately.How may this impact my birth choices?
Your midwife and doctor will discuss your choices with you. Your choices will depend on whether the breech presentation is diagnosed during late pregnancy or in labour.What will this mean for future pregnancies? How can I reduce my risk of this happening again?
If your baby is born by caesarean birth, this may impact on future pregnancies.Where can I find out more information about this condition?
Preparing for birth
Preparing for birth
 Towards the end of pregnancy, you may feel a variety of different emotions as the birth becomes closer. You may feel excited, anxious or even scared – this is all normal. There are things that you can do to help you prepare for birth.
Towards the end of pregnancy, you may feel a variety of different emotions as the birth becomes closer. You may feel excited, anxious or even scared – this is all normal. There are things that you can do to help you prepare for birth.
External cephalic version (ECV)
External cephalic version (ECV)
 This is a procedure in which a doctor, or specialist midwife attempts to the turn the baby into the correct position using gentle pressure on your abdomen with their hands.
ECV is successful in about 50% of women and is generally safe. One in every 200 babies will need to be delivered by emergency caesarean after an ECV, and your baby will be monitored before and after the procedure to ensure they remain well.
This is a procedure in which a doctor, or specialist midwife attempts to the turn the baby into the correct position using gentle pressure on your abdomen with their hands.
ECV is successful in about 50% of women and is generally safe. One in every 200 babies will need to be delivered by emergency caesarean after an ECV, and your baby will be monitored before and after the procedure to ensure they remain well.
Moxibustion for breech babies
This is a traditional Chinese technique which can be used to turn breech babies. It is done by burning a moxa-stick (a tightly packed tube of dried herbs) between the toes from 34-36 weeks of pregnancy. It has no known negative side effects and evidence suggests it can be successful at turning a breech baby. You can ask your midwife or local acupuncturist for more information.
NHS External Cephalic Version (for Breech Baby)
Your baby’s position
Your baby’s position
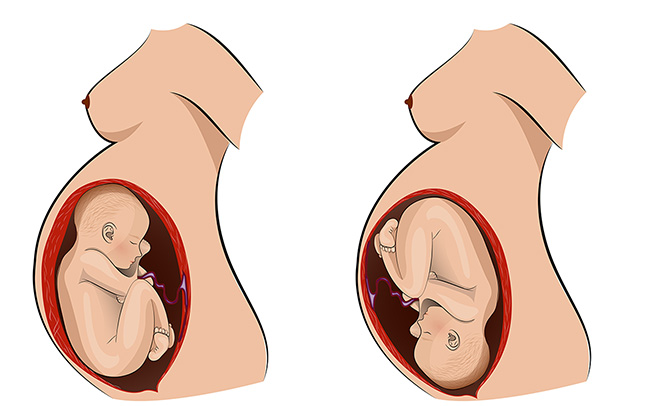
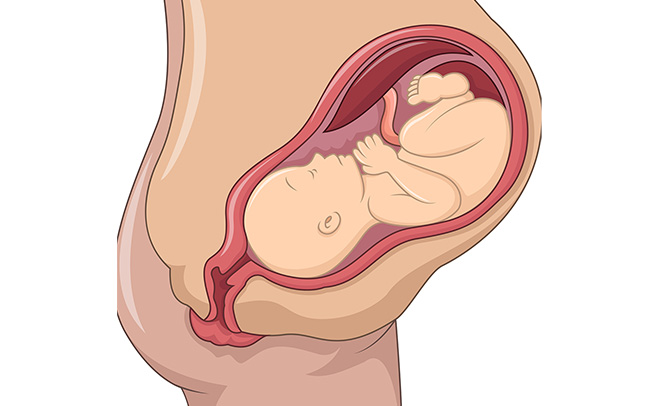 From 36 weeks pregnant, your baby should turn to the head down (cephalic) position in preparation for birth.
A small number of babies will not be in this position, and may be either breech (bottom first) or transverse/oblique (lying sideways across your abdomen). If your midwife suspects that your baby is not in the head down position, you may be offered a scan and appointment with a doctor/specialist midwife to discuss your options. These options can include either attempting to turn your baby (see related links below), vaginal breech birth or planned caesarean birth.
If your baby isn’t head down, don’t worry – there are many options available to you and your team will help you to make any decisions regarding your care moving forward.
Find out more about vaginal breech birth by reading:
From 36 weeks pregnant, your baby should turn to the head down (cephalic) position in preparation for birth.
A small number of babies will not be in this position, and may be either breech (bottom first) or transverse/oblique (lying sideways across your abdomen). If your midwife suspects that your baby is not in the head down position, you may be offered a scan and appointment with a doctor/specialist midwife to discuss your options. These options can include either attempting to turn your baby (see related links below), vaginal breech birth or planned caesarean birth.
If your baby isn’t head down, don’t worry – there are many options available to you and your team will help you to make any decisions regarding your care moving forward.
Find out more about vaginal breech birth by reading:
