Giving birth to your breech baby: Frequently asked questions
How is the diagnosis made?
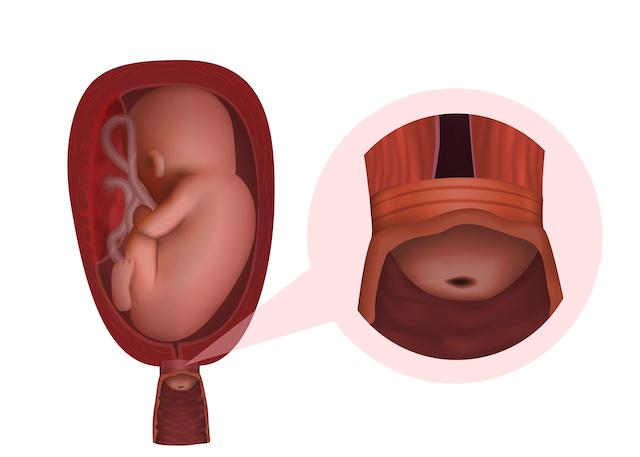
It may be suspected that your baby is lying feet or bottom first in the womb, when a midwife or obstetrician feels your abdomen at or after 36 weeks of pregnancy. This is then usually confirmed by an ultrasound scan. If you are in labour when this is suspected, the baby’s position may be confirmed by internal examination.What will the medical team recommend?
When a baby is in a breech position after 36 weeks of pregnancy there are three options that might be possible: 1. An external cephalic version (ECV) – using pressure on your abdomen to turn the baby head first 2. A planned vaginal breech birth 3. A planned caesarean birth If the breech position is first noted during labour an ECV may not be possible, and a woman will need to choose between a vaginal breech birth and a caesarean birth.What tests will/may be considered? How often may they be needed?
An ultrasound to check on the growth of your baby may be arranged if the breech position is detected before labour. This can help to guide your decision making about your preferred mode of birth.What symptoms and signs should I be looking out for?
You should contact your maternity unit if you think your waters have broken or you are in labour with a baby known to be in the breech position.What are the ‘red flag’ symptoms/concerns, which means that they should be reported immediately?
If your waters break and your baby is lying feet or bottom first, there is an increased chance of the umbilical cord being below the baby – this is called an umbilical cord prolapse. If this happens you should promptly attend the hospital for review. If a loop of cord is seen outside the vagina, then you should call 999 immediately.How may this impact my birth choices?
Your midwife and doctor will discuss your choices with you. Your choices will depend on whether the breech presentation is diagnosed during late pregnancy or in labour.What will this mean for future pregnancies? How can I reduce my risk of this happening again?
If your baby is born by caesarean birth, this may impact on future pregnancies.Where can I find out more information about this condition?
Early pregnancy concerns
Early pregnancy concerns

Cervical insufficiency (incompetence)
Cervical insufficiency (incompetence)
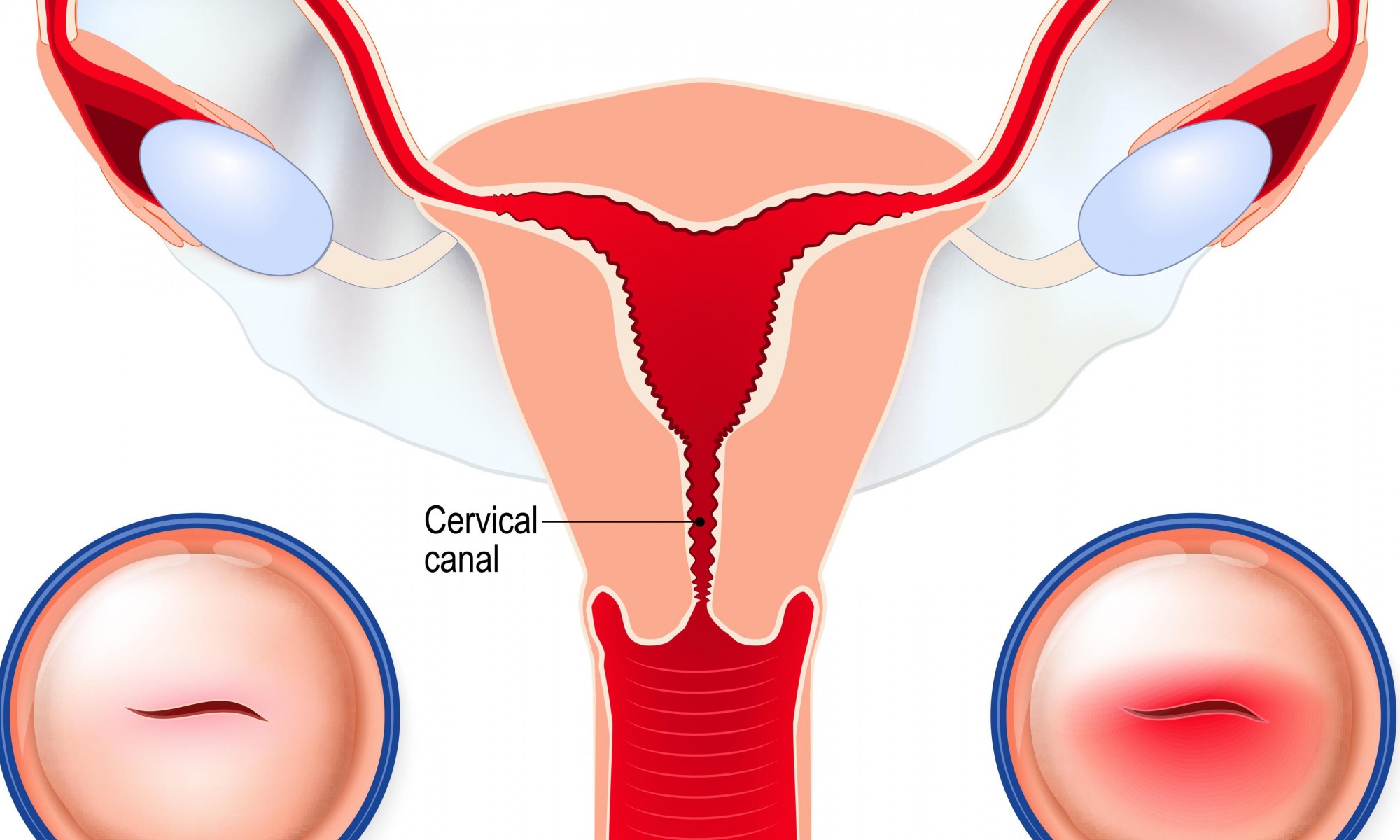
 In some women, the muscles that surround the neck of the womb (cervix) are weaker than usual. This is known as cervical insufficiency, cervical incompetence or short cervix. Previous surgery or investigations to this area can sometimes cause the cervix to open too early, leading to miscarriage or pre-term birth. Cervical insufficiency can also be something you can be born with due to the shape of the uterus.
The mid-trimester ultrasound scan will usually identify a short or weak cervix. Your doctor may want to check your cervix early in pregnancy if you have had several miscarriages or if you have had a baby born before 37 weeks of pregnancy.
In some women, the muscles that surround the neck of the womb (cervix) are weaker than usual. This is known as cervical insufficiency, cervical incompetence or short cervix. Previous surgery or investigations to this area can sometimes cause the cervix to open too early, leading to miscarriage or pre-term birth. Cervical insufficiency can also be something you can be born with due to the shape of the uterus.
The mid-trimester ultrasound scan will usually identify a short or weak cervix. Your doctor may want to check your cervix early in pregnancy if you have had several miscarriages or if you have had a baby born before 37 weeks of pregnancy. Cervical erosion (ectropion)
Cervical erosion (ectropion)
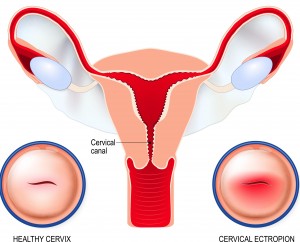 Cervical ectropion (cervical erosion) occurs when the soft cells that line the inside of the cervical canal spread to the outer surface of your cervix.
These cells are redder and are more sensitive than the cells typically on the outside, which is why they may cause symptoms like bleeding and discharge.
Cervial ectropion can be caused by hormonal changes, pregnancy and being on the pill. During pregnancy it usually resolves on its own but since it can sometimes cause bleeding, it is advisable to seek advice from your midwife or maternity triage department to rule out any other cause for the bleeding.
Cervical ectropion (cervical erosion) occurs when the soft cells that line the inside of the cervical canal spread to the outer surface of your cervix.
These cells are redder and are more sensitive than the cells typically on the outside, which is why they may cause symptoms like bleeding and discharge.
Cervial ectropion can be caused by hormonal changes, pregnancy and being on the pill. During pregnancy it usually resolves on its own but since it can sometimes cause bleeding, it is advisable to seek advice from your midwife or maternity triage department to rule out any other cause for the bleeding. Early pregnancy symptoms and feelings
Early pregnancy symptoms and feelings
 Early pregnancy comes with a range of physical symptoms and mixed emotions (feelings), some of which may begin before you have a positive pregnancy test.
These include:
Early pregnancy comes with a range of physical symptoms and mixed emotions (feelings), some of which may begin before you have a positive pregnancy test.
These include:
- sore (sensitive), heavy breasts
- nausea or vomiting
- tiredness or sleeplessness
- needing to pass urine more often
- light spotting or bleeding, sometimes accompanied by mild stomach cramps
- a feeling of stretching and pulling in the tummy (abdomen) and back and at the tops of your legs
- backache
- feeling bloated with excess gas (wind)
- diarrhoea or constipation
- headaches
- dizziness or feeling lightheaded
Giving birth to your breech baby
Giving birth to your breech baby
 About one in 25 babies are in a breech position (bottom first or feet first) after 36 weeks of pregnancy. If your baby remains breech, you should be offered the choice of attempting to turn your baby, planning a caesarean birth or planning a vaginal birth. The most likely outcome, no matter what you choose, is that you and your baby will be well. But it’s important for you to consider the benefits and risks of each option for you.
Turning the baby head-down gives you the greatest chance of a vaginal birth, about 80%. The procedure of attempting to turn a breech baby is known as External Cephalic Version (ECV). If baby remains breech, only about 60% of these babies will be born vaginally. Some will require a pre-labour caesarean birth, and some will require a caesarean delivery in labour.
All women with a baby who remains breech are offered the option of a planned caesarean birth at 39 weeks. That is because we can identify a difference in short-term outcomes for breech babies. Following a caesarean birth, the perinatal mortality (death) rate is reduced, at 0.5 in 1,000, compared to 1 in 1,000 following a head-first birth, and 2 in 1,000 following a breech birth. In the short-term, there is also an increased chance your baby could need special care following a vaginal birth. However, by two years of age, the same studies show no difference between planning a caesarean birth and planning a vaginal birth for a breech baby.
The benefits of planning a vaginal birth include a quicker recovery and avoidance of the risks associated with caesarean surgery. These include things like heavy bleeding and infection. A caesarean scar also introduces some additional risks, for mother and baby, in all future pregnancies. The perineal outcomes (remaining intact) are similar or better following vaginal breech births, compared to head-first births, and there are fewer instrumental deliveries. You should have the same choice of pain relief, and freedom to choose your birthing position, as you would in any birth. But some of this may depend on the experience of your team, so you should discuss it with them.
Your doctor or specialist midwife will be able to provide you with more information about some specific clinical situations that make breech births safe or less safe, and whether these apply to you. The most important factor that influences the safety of vaginal breech birth is the training, skill and experience of the professionals attending the birth. If your hospital is unable to provide you with a skilled attendant, and you would like to consider planning a vaginal breech birth, you should be offered a referral to a hospital that can.
About one in 25 babies are in a breech position (bottom first or feet first) after 36 weeks of pregnancy. If your baby remains breech, you should be offered the choice of attempting to turn your baby, planning a caesarean birth or planning a vaginal birth. The most likely outcome, no matter what you choose, is that you and your baby will be well. But it’s important for you to consider the benefits and risks of each option for you.
Turning the baby head-down gives you the greatest chance of a vaginal birth, about 80%. The procedure of attempting to turn a breech baby is known as External Cephalic Version (ECV). If baby remains breech, only about 60% of these babies will be born vaginally. Some will require a pre-labour caesarean birth, and some will require a caesarean delivery in labour.
All women with a baby who remains breech are offered the option of a planned caesarean birth at 39 weeks. That is because we can identify a difference in short-term outcomes for breech babies. Following a caesarean birth, the perinatal mortality (death) rate is reduced, at 0.5 in 1,000, compared to 1 in 1,000 following a head-first birth, and 2 in 1,000 following a breech birth. In the short-term, there is also an increased chance your baby could need special care following a vaginal birth. However, by two years of age, the same studies show no difference between planning a caesarean birth and planning a vaginal birth for a breech baby.
The benefits of planning a vaginal birth include a quicker recovery and avoidance of the risks associated with caesarean surgery. These include things like heavy bleeding and infection. A caesarean scar also introduces some additional risks, for mother and baby, in all future pregnancies. The perineal outcomes (remaining intact) are similar or better following vaginal breech births, compared to head-first births, and there are fewer instrumental deliveries. You should have the same choice of pain relief, and freedom to choose your birthing position, as you would in any birth. But some of this may depend on the experience of your team, so you should discuss it with them.
Your doctor or specialist midwife will be able to provide you with more information about some specific clinical situations that make breech births safe or less safe, and whether these apply to you. The most important factor that influences the safety of vaginal breech birth is the training, skill and experience of the professionals attending the birth. If your hospital is unable to provide you with a skilled attendant, and you would like to consider planning a vaginal breech birth, you should be offered a referral to a hospital that can.
Pregnancy matters
Pregnancy matters

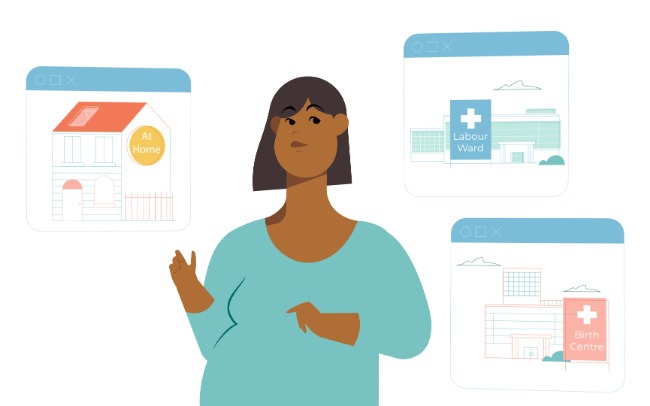
Options for place of birth
Options for place of birth
Place of birth choices
You can discover where you can give birth according to your preferences and needs – in a labour ward, in a birth centre or at home.
Watch the video to learn about the different options. Your midwife at your chosen maternity unit or your doctor can help advise you on the best choice for you.
Video credit: NHS North West London maternity services.